Yellow fever is an infectious disease caused by a virus Flavivirus, a genus to which the viruses responsible for Dengue and Japanese Encephalitis also belong. The first report of an epidemic dates back to 1648 and occurred in Mexico, in the Yucatan Peninsula. The name "yellow fever" was first used during an epidemic in the Barbados Islands in 1750. The disease became a major problem at the time of colonialism and travel between Africa and South America in the 1700s, so much so that manifestations of it were reported in several European and American ports at that time.
This disease primarily affects humans and monkeys and is transmitted through the bite of Aedes aegypti mosquitoes. Mosquitoes generally bite during daylight hours. Those most at risk are all those who frequent, for work or tourism, forest or jungle areas in countries where the disease is present. A sylvatic cycle and an urban cycle are possible, so the disease may also be present in the suburbs of cities. Yellow fever is endemic in tropical areas of Africa and South America, where epidemics can also occur. Transmission can occur at altitudes up to 2,300 meters in South America and at even higher altitudes in Africa. Some countries may not report cases simply because there is a high level of yellow fever vaccination coverage in the population or because epidemiological surveillance is very poor. It is estimated that yellow fever causes 200,000 infections and about 30,000 deaths each year, 90 percent of them in Africa. Nearly one billion people live in countries around the world where the disease is present, such as tropical areas of South America and Africa. Yellow fever is not present in Asia.
The incubation period of yellow fever, between infection and the onset of symptoms is generally 3 to 6 days. Most people infected with the virus are asymptomatic or develop only mild symptoms that leave no sequelae. Symptoms are represented by: sudden-onset fever, chills, asthenia, headache, lower back pain, arthralgias, nausea, vomiting.
The majority of people infected with the virus are asymptomatic.
Most symptoms recede within a week, but asthenia may persist for several months. In about 15% of individuals who develop symptoms, a severe form of the disease can occur, which exits in death in 30-60% of cases. In nonimmune travelers and during an outbreak in areas that usually experience low levels of virus circulation, the lethality rate can exceed 50%.
Given the risk of evolution into a severe form, all individuals with symptoms should always undergo specialized medical evaluation.
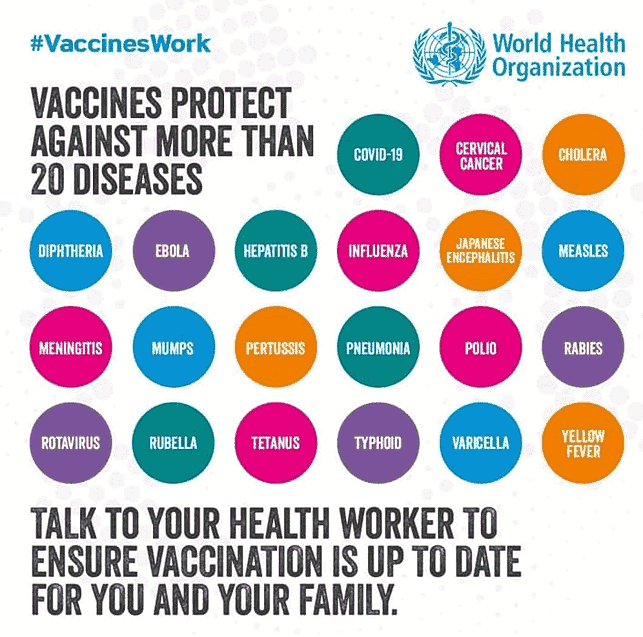
Since there is no specific therapy for this disease, vaccination is always recommended. Another recommendation is the use of mosquito repellents to be put directly on the skin and clothing during periods of contact or when crossing risky environments (safari, jungle or forest excursions, etc.)
The yellow fever vaccination
.The vaccine is administered subcutaneously through a single 0.5 ml injection in adults and children from 9 months of age.
Precautions to the administration of the vaccine include ages 6 to 9 months and ages over 60 years (due to the increasing risk of major side effects) as well as pregnancy and lactation.
The vaccine must be administered at least ten days before exposing oneself to the risk of yellow fever infection. This is because at least ten days are required to provide good protection against the virus.
The previous requirement in the International Health Regulations for a booster at ten years after the previous administration has been corrected to indicate that the protection conferred by the vaccine lasts a lifetime. The second dose of the yellow fever vaccine should be considered as a second chance for seroconversion and could be applied to particular categories of fragile or at-risk individuals including very young children, pregnant women, hematopoietic stem cell transplant recipients, and HIV-positive individuals.
The second dose of the yellow fever vaccine should be considered as a second chance for seroconversion and could be applied to particular categories of fragile or at-risk individuals including very young children, pregnant women, hematopoietic stem cell transplant recipients, and HIV-positive individuals.
There is no evidence that inactivated vaccines interfere with the immune response to yellow fever vaccine. Therefore, inactivated vaccines (hepatitis A and B, diphtheria-tetanus-pertussis, meningitis) can be administered at the same time or at any time before or after yellow fever vaccination. In cases where the YF vaccine is administered in a session that also includes other vaccinations, the rule of thumb always applies to use different limbs if possible or, in the case of using the same limb, to respect the minimum distance of 2.5 cm between inoculation sites.
Yellow fever vaccination is not only recommended but is mandatory before traveling to the following countries:
.Angola, Benin, Burkina Faso, Burundi, Cameroon, Democratic Republic of Congo, Ivory Coast, Gabon, Ghana, Guinea Bissau, French Guiana, Liberia, Mali, Niger, Central African Republic, Rwanda, Sao Tome and Principe, Sierra Leone, Togo.
Where to check the need for vaccination in real time
.Consult the WHO website, at the international travel page and the yellow fever-specific page, where year-by-year updates on countries requiring yellow fever vaccination are documented.
Where you can get the yellow fever vaccination
.Vaccination can be requested at centers authorized by the Ministry of Health. All Local Health Authorities have set up clinics for international travelers where both recommended and mandatory vaccinations such as yellow fever for some countries can be requested.
Sources:
Various authors. Yellow Fever: the disease and vaccine prevention. EDRA Milan, 2020
.